|
The numbers surrounding mental health disorders and mental illness
are staggering. One in four adults 57 million) experience a mental
health disorder in a given year. One in 17 lives with a serious mental
illness such as schizophrenia, major depression, or bipolar disorder.
One in 10 children live with a serious mental or emotional disorder.
Never in our history have we known so much about mental health and
how to enable people with mental illnesses to live, work, learn, and
participate fully in society. Recovery from mental illness is now a
realistic hope. Yet, much of what we know is not accessible to the
people who need it most. “Simply put, treatment works, if you can get
it. But in America today, it is clear that many people living with
mental illness are not provided with the essential treatment they need”,
says Michael J. Fitzpatrick, executive director of the National Alliance
on Mental Illness.
Lack of treatment is often caused by several factors.
Budget cuts causing the reduction or elimination of programs, mental
health not being a public priority, stigma of mental disorders, lack of
knowledge of signs and risk factors.
A survey released by the American Psychiatric Association (APA) found
a significant lack of consumer knowledge concerning the warning signs,
causes, and effective treatments for mental illnesses. 44 percent
reported knowing almost nothing about mental illnesses. But asked
whether they would benefit from knowing more about the warning signs of
mental illness, 84 percent said yes.
|
- The Basics Defined:

- Psychosocial Health:
- A multidimensional term that encompasses the mental,
emotional, social, and spiritual dimensions of health.
- Each dimension of Psychosocial Health is a part of who
we are. Influencing factors include:
- External Factors:
- Family and friends
- Personal experience
- Internal Factors:
- Heredity
- Hormonal function
- Physical fitness
- Self-Efficacy and Self-Esteem:
- Self-Efficacy: Belief in one’s own ability
- Self-Esteem: Sense of self-respect
- Learned Helplessness vs. Optimism(Seligman)
- Learned helplessness:
- A behavioral state and personality trait of
a person who believes that he or she is
ineffectual, or his or her responses are futile.
- A response to continued failure where people
give up and fail to take action to help
themselves.
- Learned optimism:
- The idea that an optimistic approach can be
cultivated. developed, or learned.
- Learning optimism is done by consciously
challenging negative thoughts, and talking
oneself through personal setbacks or defeat.
- Personality:
- Unique set of characteristics developed by a
person's heredity, culture, environment.
- Psychosocially healthy people:
- Feel good about themselves and have a sense of
contentment.
- Feel comfortable with other people.
- Have the ability to deal with stress and bounce back
from adversity.
- Are able to meet the demands of life.
- Manage personal feelings and deal with difficulties
in a positive manner.
- Enrich the lives of others.
- Cherish the things that make them happy.
- Maintain a balance between work and play, rest and
activity, etc.
- Appreciate and respect nature.
- Have the ability to build and maintain fulfilling
relationships.
- Mental Health:

- Describes the "thinking" part of psychosocial health.
- The ability to reason, interpret, and remember from
a unique and personal perspective.
- To intellectually process information, attach
meaning, and make decisions.
- To think rationally with fairly accurate perceptions
of events; learn from setbacks
- Emotional Health:
- Describes the "feeling" part of psychosocial health.
(Emotions are intensified feelings or complex patterns of
feelings that we all experience.)
- To maintain control of emotions and their behavior.
- To handle life’s challenges, build strong
relationships, and recover from setbacks.
- To respond in a stable and appropriate manner to
upsetting events
- Social Health:
- Describes our interactions with others and the ability
to adapt to various social situations.
- The ability to interact in a positive manner the
with people around us, either personally or in a group
setting.
- The ability to make friends easily and work with
people in a friendly manner.
- The ability to:
- Listen and express oneself when appropriate
- Form healthy relationships
- Act in a socially acceptable and
responsible way.
- Find a best fit for themselves in society.
- Spiritual Health:
- Describes an individual's sense of peace, purpose,
connection to others, and beliefs about the meaning of life.
- Refers to the sense of belonging to something
greater than the purely physical or personal dimensions
of existence.
- Behaviors often associated with wellness are key
components of a healthy spiritual life. Examples include
- Volunteerism
- Social responsibility
- Optimism
- Contributing to society
- Connectedness with others
- Feeling of belonging/being part of a group
- A reason to care for self.

- Psychosocial Disorders and
Illness:
- Mood Disorders:
- Depression:
- Defined:
- Depression is a common but serious mental illness
typically marked by prolonged periods of sad or anxious
feelings.
- Most college students occasionally feel sad or
anxious, but these emotions usually pass quickly—within
a couple of days.
- Untreated depression lasts for a long time,
interferes with day-to-day activities and is much more
than just being “a little down” or “feeling blue.”
- Women are 70% more likely than men to
experience depression during their lifetime. (NIMH)
- Cause(s) of Depression:
- Depression does not have a single cause, however,
there are factors can lead to depression, including:
- Genetics
- Environment:
- Surroundings and life experiences, such as
stress, also affect the risk for depression.
- Stresses of college may include:
- Living away from family for the first
time
- Missing family or friends
- Feeling alone or isolated
- Experiencing conflict in relationships
- Facing new and sometimes difficult
school work
- Worrying about finances.
- Types of Depression:
- Major Depressive Disorder or Major Depression:
- Characterized by the inability to enjoy life and
experience pleasure.
- The symptoms are constant, ranging from moderate
to severe. Left untreated, major depression
typically lasts for about six months.
- People with this disorder may have only one
episode of major depression in their lifetimes. But
more often, depression comes back repeatedly.
- There are many things you can do to support your
mood and reduce the risk of recurrence.
- Dysthymic Disorder or Dysthymia:
- Dysthymia is mild, chronic depression. The
symptoms of dysthymia last for a long time, often 2
years or more.
- Dysthymia is less severe than major depression,
but it can still interfere with everyday activities.
- People with dysthymia may also experience one or
more episodes of major depression during their
lifetimes.
- Seasonal Affective Disorder (SAD):
- Characterized by the onset of depression during
the winter months, when there is less natural
sunlight, and lifts during spring and summer.
- SAD may be effectively treated with light
therapy, antidepressant medication, or
psychotherapy.
- Common Signs and Symptoms:
- The symptoms of depression vary. If you are
depressed, you may feel:
- Sad or Anxious
- Empty or Hopeless
- Guilty
- Worthless or Helpless
- Irritable or Restless.
- You may also experience one or more of the
following:
- Loss of interest in activities you used to enjoy
- Lack of energy
- Problems concentrating, remembering information,
or making decisions
- Problems falling sleep, staying asleep, or
sleeping too much
- Loss of appetite or eating too much
- Aches, pains, headaches, cramps, or digestive
problems that do not go away.
- Thoughts of suicide or suicide attempts.
- Types of Treatment:
- Medication:
- Antidepressants primarily work on brain
chemicals called neurotransmitters, especially
serotonin and norepinephrine.
- Other antidepressants work on the
neurotransmitter dopamine.
- Scientists have found that these particular
chemicals are involved in regulating mood, but they
are unsure of the exact ways that they work.
- The latest information on medications for
treating depression is available on the
U.S. Food and Drug Administration (FDA) website.
- Psychotherapy:
- Often referred to as "talk therapy", the two
main types of psychotherapies include:
- Cognitive-behavioral therapy (CBT): therapy
based on the idea that thoughts guide feelings
and behaviors; by changing the way we think
will, in turn, change the way we feel and/or
act.
- Interpersonal therapy (IPT): short-term
supportive psychotherapy that focuses on a
person's psychiatric symptom in a social,
relationship context, and the improvement of
interpersonal functioning.
- Electroconvulsive therapy and other brain
stimulation therapies:
- Also known as "shock therapy," it is used with
cases of severe depression when other treatments
have not worked.
- Bipolar Disorder:
- Also known as manic depression, bipolar disorder
causes serious shifts in mood, energy, thinking, and
behavior–from the highs of mania on one extreme, to the lows
of depression on the other.
- Attention Deficit Hyperactivity
Disorder (ADHD):
- ADHD is one of the most common childhood disorders and
can continue through adolescence and adulthood.
- Symptoms include difficulty staying focused and paying
attention, difficulty controlling behavior, and
hyperactivity (over-activity).

- Three Subtypes of ADHD:
- Predominantly Hyperactive-Impulsive:
- Most symptoms (six or more) are in the
hyperactivity-impulsivity categories.
- Fewer than six symptoms of inattention are
present, although inattention may still be present
to some degree.
- Predominantly Inattentive:
- The majority of symptoms (six or more) are in
the inattention category and fewer than six symptoms
of hyperactivity-impulsivity are present, although
hyperactivity-impulsivity may still be present to
some degree.
- Children with this subtype are less likely to
act out or have difficulties getting along with
other children. They may sit quietly, but they are
not paying attention to what they are doing.
Therefore, the child may be overlooked, and parents
and teachers may not notice that he or she has ADHD.
- Combined Hyperactive-Impulsive and Inattentive:
- Six or more symptoms of inattention and six or
more symptoms of hyperactivity-impulsivity are
present.
- Most children have the combined type of ADHD.
- Treatments can relieve many of
the disorder's symptoms, but there is no cure. With
treatment, most people with ADHD can be successful in school
and lead productive lives. Researchers are developing more
effective treatments and interventions, and using new tools
such as brain imaging, to better understand ADHD and to find
more effective ways to treat and prevent it.
- Anxiety Disorders:
- The persistent feelings of threat and anxiety about
everyday problems of living. They include:
- Generalized Anxiety Disorder:
- Involves excessive worry and anxiety that
interferes with normal living.
- Obsessive-Compulsive Disorder:
- Obsessive-compulsive disorder (OCD) is an
anxiety disorder characterized by uncontrollable,
unwanted thoughts and repetitive, ritualized
behaviors you feel compelled to perform.
- Obsessions are involuntary, seemingly
uncontrollable thoughts, images, or impulses that
occur over and over again in your mind.
- Compulsions are behaviors or rituals that
you feel driven to act out again and again.
- Phobias:
- Deep persistent fears of objects, activities, or
situations.
- Panic Attacks:
- Sudden onsets of disabling terror.
- Symptoms can can often mimic those of a heart
attack
- Post-traumatic stress disorders:
- Personality Disorders:
- Personality disorders are a group of psychiatric
conditions in which a person's long-term (chronic)
behaviors, emotions, and thoughts are very different from
their culture's expectations and cause serious problems with
relationships and work.
- Common types of personality disorders include:
- Paranoid Personality Disorder: pervasive, unfounded
suspicion and mistrust of other people, irrational
jealousy, and secretiveness.
- Narcissistic Personality Disorder: exaggerated sense
of self-importance and self-absorption.
- Borderline Personality Disorder: impulsiveness and
engaging in risky behaviors
- Schizophrenia:
- Schizophrenia is a biological disease of the brain, characterized by the alteration of senses; the inability
to sort out incoming stimuli and to make appropriate
responses; an altered sense of self; and radical changes in
emotions, movements, and behaviors.
- Victims of this disease may not be able to
function in society.
- It is treatable, but not curable.
- Treatments
include hospitalization, medication, and supportive therapy.
- Suicide:

- More than 36,000 people in the United States die by suicide
every year; our country's 10th leading cause of death.
- It is often characterized as a response to a single
event or set of circumstances.
- The factors that contribute to any particular suicide
are diverse and complex.
- While some suicides occur without any outward warning,
most people who are suicidal do give warnings.
- Prevent the suicide of loved ones by learning to
recognize the signs of someone at risk, taking those signs
seriously and knowing how to respond to them. Fifty to 75 percent of all suicides give some
warning of their intentions to a friend or family
member.
- Warning signs
of suicide from the AFSP include:
- Observable signs of serious depression:
- Unrelenting low mood
- Pessimism
- Hopelessness
- Desperation
- Anxiety, psychic pain and inner tension
- Withdrawal
- Sleep problems
- Increased alcohol and/or other drug use
- Recent impulsiveness and taking unnecessary risks
- Threatening suicide or expressing a strong wish to
die
- Making a plan:
- Giving away prized possessions
- Sudden or impulsive purchase of a firearm
- Obtaining other means of killing oneself such as
poisons or medications
- Unexpected rage or anger
- How to Help:
- Take imminent signs seriously.
- Show care and concern, but be direct, ask if
they are considering suicide
- Be Willing to Listen:
- Ask if they are taking any medications or seeing a
therapist.
- Offer hope, never argument.
- Seek Professional Help:
- Help the individual seek out a mental health
professional.
- In an Acute Crisis Situation:
- The primary sign of a suicide crisis situation
surrounds an individual who is talking about, or
threatening suicide.
- Call 911 or the National Suicide Prevention Lifeline
at 1-800-273-TALK (8255) immediately.
- The important thing to understand is that feeling suicidal
is not a character defect, and it doesn't mean that a person is
crazy, weak, or flawed. It only means that the person has more
pain than they feel capable of coping with.
- But help is out there. Talking openly about suicidal
thoughts and feelings can save a life. So don't wait: reach out.
- Mental Health Professionals:
- Psychiatrist:
- A medical doctor who spends up to 12 years studying
psychosocial health and disease.
- A psychiatrist is able to write prescriptions.
- Psychoanalyst:
- Usually a psychiatrist or a clinical psychologist, who
is trained in the psychoanalysis method of treating
emotional disorders.
- Psychologist:
- Usually is a Ph.D. trained in various types of therapy,
including behavior and insight therapy.
- Clinical/Psychiatric Social Worker:
- Holds a master's degree and has at least 2 years of
experience in a clinical setting.
- Licensed Mental Health Therapist or Counselor:
- Usually holds a master's degree in counseling, or
psychology, they often specialize in one type of counseling
such as family, marital, relationship, children, etc.
- Psychiatric Nurse Specialist:
- Certified by the American Nursing Association in adult,
child, or adolescent psychiatric nursing.
|
- 30 percent of college students reported feeling “so depressed
that it was difficult to function.
- Anxiety disorders affect between 20 and 30 million people.
- Military Veteran Statistics from the JED Foundation:
- Estimated 300,000 veterans and their dependents are
currently enrolled in American institutions of higher education,
representing 4 percent of the total undergraduate population.

- Military undergraduates tend to be younger than veterans in
general, but older than traditional undergraduates. In 2007–08,
some 85 percent of military undergraduates were aged 24 or
older.
- Women represented 27 percent of all military undergraduates
in 2007–08, although they made up just 7 percent of all U.S.
veterans in 2006.
- 43 percent of military undergraduates in 2007–08attended
public two-year institutions. Twenty-one percent attended public
four-year colleges. Private for-profit and private
not-for-profit four-year institutions each enrolled about
one-eighth of all military undergraduates.
- Nearly 20 percent of U.S. service members returning from
combat will report symptoms of PTSD or major depression (RAND –
rand.org).
- Only 53% of those with PTSD or depression sought help in the
past year. (RAND – rand.org).
- More than half of the estimated 300,000 military service
members who are suffering from depression, post-traumatic stress
disorders, and traumatic brain injury are going without
treatment because of the gaps in mental health care and stigma
issues. (RAND – rand.org).
- Over half of surveyed soldiers who met criteria for a
psychological health problem thought they would be perceived as
weak, treated differently, or blamed for their problem if they
sought help (DOD Task Force on MH).
- 90% of today’s seriously wounded U.S. military service
members are surviving (VA).
-
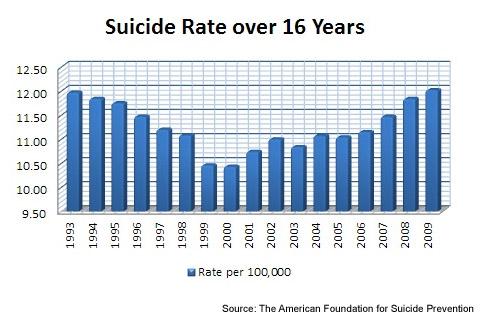
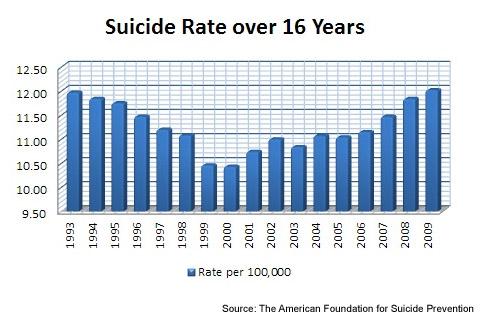 Suicide
Statistics from the American Foundation for Suicide Prevention: Suicide
Statistics from the American Foundation for Suicide Prevention:
- The latest data available from the Centers for Disease
Control and Prevention indicates that 36,909 suicide deaths were
reported in the U.S. in 2009.
- This latest rise places suicide again as the tenth
leading cause of death in the U.S.
- Nationally, the suicide rate increased 2.4 percent over
2008 to equal approximately 12.0 suicides per 100,000
people.
- The rate of suicide has been increasing since 2000. This
is the highest rate of suicide in fifteen years.
- Every 14.2 minutes someone in the United States dies by
suicide.
- Nearly 1,000,000 people make a suicide attempt every year.
- 90% of people who die by suicide have a diagnosable and
treatable psychiatric disorder at the time of their death.
- Most people with mental illness do not die by suicide.
- Recent data puts yearly medical costs for suicide at nearly
$100 million (2005).
- Men are nearly 4 times more likely to die by suicide than
women. Women attempt suicide 3 times as often as men.
- Suicide rates are highest for people between the ages of 40
and 59.
- White individuals are most likely to die by suicide,
followed by Native American peoples.
- Fifty to 75 percent of all suicides give some warning of
their intentions to a friend or family member.
- In a national survey by the McKinsey Global Institute and
International Data Corp concerning email:
- The average employee spends 28 percent of a normal work day
reading, writing or responding to email, which amounts to:
- 2 hours and 14 minutes daily
- 13 hours in an average workweek
- 78 days of work in the average year
- The average monthly time a person spends on a Facebook per
month.
- 441 minutes monthly on Facebook mobile app
- 391 minutes monthly on the Facebook classic website.
|
|
What is Your Emotional Intelligence?
Emotional intelligence (EQ) is the ability to identify, use,
understand, and manage emotions in positive ways to relieve stress,
communicate effectively, empathize with others, overcome challenges, and
diffuse conflict. Emotional intelligence impacts many different aspects
of your daily life, such as the way you behave and the way you interact
with others. If you have a high emotional intelligence you are able to
recognize your own emotional state and the emotional states of others
and engage with people in a way that draws them to you. You can use this
understanding of emotions to relate better to other people, form
healthier relationships, achieve greater success at work, and lead a
more fulfilling life.
Attributes of Emotional Intelligence:
- Self-Awareness:
- Do you recognize your own emotions and how they affect your
thoughts and behavior?
- Do you know your strengths and weaknesses?
- Do you have self-confidence?
- Self-Management:
- Are you able to control impulsive feelings and behaviors?
- Can you manage your emotions in healthy ways?
- Do you take initiative?
- Do you follow through on commitments?
- Do you adapt to changing circumstances?
- Social Awareness:
- Can you understand the emotions, needs, and concerns of
other people?
- Do you pick up on emotional cues?
- Do you feel comfortable socially?
- Can you recognize the power dynamics in a group or
organization?
- Relationship Management:
- Do you know how to develop and maintain good relationships?
- Can you communicate clearly?
- Do you inspire and influence others?
- Can you work well in a team?
- Can you manage conflict?
|
|
Thoughts for Living |
 |
|
Studies show that positive emotions can cancel out
stress-related risks associated with heart disease, cancer, and
the aging process. So how do you get happy? Consider the
following:
- Understand that Physical Health is Tied to
Psychosocial Health:

- Focus on Sleep, 7 to 8 hours nightly.
- Learn about good nutrition and eat for wellness.
- Exercise to relieve stress, enhance mood, and build
a stronger sense of self.
- Sunlight daily, 10 to 15 minutes daily, when
possible.
- Eliminate life's hazards (alcohol, tobacco, drugs)
- Do Things that Positively Impact Others.
- Being useful to others and being valued for what you
do can help build self-esteem.
- Thank You Letters for Wellness:
- When Psychology students at the University of
Michigan wrote a series of one-page thank-you letters
every 2 weeks for 6 total weeks, measurements showed a
significant mood-boost in the writers.
- After the assignment the instructor says his
students feel happier "100 percent of the time."
- Every month, try writing a couple of thank-you notes
to people who did something nice for you.
- Seeing the world through the rose-colored lenses of
appreciation and thankfulness can help boost feelings of
life satisfaction and overall well-being, and that is
great for your health.
- Practice Self-discipline:
- Self-control naturally leads to a sense of
hopefulness and can help you overcome despair,
helplessness, and other negative thoughts.
- Enjoy the Beauty Around You:
- Studies show that simply walking through a garden
can lower blood pressure and reduce stress.
- The same goes for strolling through a park or an art
gallery, hiking, admiring architecture, or sitting on a
beach.
- Manage Your Stress Levels:
- Stress takes a heavy toll on mental and emotional
health, so it’s important to keep it under control.
- While not all stressors can be avoided, stress
management strategies can help you bring things back
into balance.
- Meditate. It eases stress, strengthens immunity, and
ups happiness.
- Limit Negative Thoughts:
- Avoid being absorbed by repetitive mental habits.
- Negative thoughts about yourself, other people, or
the world around you suck up time, drain your energy,
and trigger feelings of anxiety, fear, and depression.
- Understand Unhappiness:
- When it happens, why it happens, and if it was in
your control.
- Learn from it, it’s a chance for you to make
positive changes.
- Make Leisure Time a Priority.
- Do things for no other reason than that it feels
good to do them.
- Go to a funny movie, take a walk on the beach,
listen to music, read a good book, or talk to a friend.
- Doing things just because they are fun is no
indulgence, play is an emotional and mental health
necessity.
- Stop and Look Around:
- True happiness often shows itself when a person
takes an honest look at the gifts that they posses, and
the people in their lives.
|
Mental health issues are on
the rise on college campuses
across the country. Better
and accessible screening as
well as earlier diagnosis of
mental health conditions are
critical to getting quality
treatment and improving
one's quality of life. This
has allowed more students
with mental health
conditions to go on to
college and be successful.
Living in a new environment
outside the familiarity of
home can create overwhelming
and stressful circumstances.
College students can greatly
benefit from understanding
that a certain amount of
stress is normal, but that
too much stress can be
unhealthy and unproductive.
Knowing the signs of stress,
its causes and how to manage
it can be a great tool in
promoting and preserving
good mental health.
Click on the links
below for information about
common issues facing college
students:
|
 |
|






 Suicide
Statistics from the American Foundation for Suicide Prevention:
Suicide
Statistics from the American Foundation for Suicide Prevention: